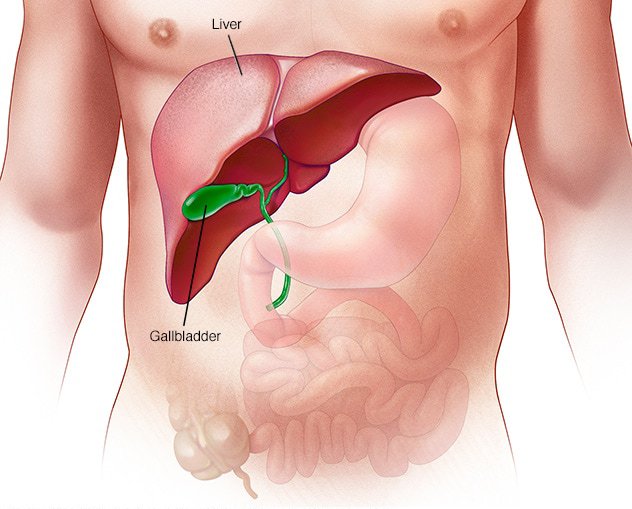
Liver a dark reddish-brown, large lobed glandular organ in the abdomen. It is located just under your rib cage on the right side of your abdomen.
Liver is of the utmost importance for the survival of an individual, it has many tasks and several critical functions to perform including:
• Nutrient, hormone, and medication processing.
• Producing bile, which help the body absorb fats, cholesterol, and fat-soluble vitamins.
• Removing degradation products of normal body metabolism.
• Removing bacteria and toxins from the blood, controlling excessive bleeding.
• Preventing infections and regulating immune responses.
• Processes Glucose and regulating sugar.
A liver transplant is a surgical procedure in which a failing or diseased liver is removed and replaced with a healthy liver. It can be a whole liver from a deceased donor or a part of liver from living donor. A divided liver can regrow to full size in both, the body of the recipient and the body of the living donor.
A liver transplant is recommended as an option for people suffering from various types of severe complications caused by chronic liver disease. In rare cases where a previously healthy liver suddenly stops functioning, a liver transplant is also considered a treatment option.
People who require liver transplants typically suffer from one or more of the following conditions:
Hepatitis B and Hepatitis C, Alcoholic liver disease, Non-alcoholic fatty liver disease, Genetic diseases affecting liver such as hemochromatosis and Wilson’s disease, and Diseases affecting the bile ducts can be some of the major causes of cirrhosis that lead to liver failure.
Ther are three type of organ donor:
Please note that only 'near relative' such as spouse, parents, siblings, grandparents, and children of the recipient can be living donors for liver transplant as per the law in several countries.
Here are brief details of what happen before, during and after liver transplant.
Once a liver transplant is recommended by your doctor, you'll need to choose transplant centre where you will be evaluated to see if you meet eligibility requirements of that particular transplant centre. As a result, you may need to be evaluated to determine whether you are healthy enough to have transplant surgery, whether you have any medical conditions that could interfere with the transplant, and whether you are willing to take the necessary medications. After the evaluation is done, you will undergo specific tests and procedures, which includes:
Doctors will evaluate the results of your tests to determine the severity of your illness and the urgency with which you require a liver transplant.
Doctors look into following factors to identify a suitable and compatible liver:
Having a compatible blood type reduces the likelihood of your body rejecting the donor liver. Sharing a similar body size increases the likelihood that your new liver will be the correct size for your body. Being in the same geographical region also helps to ensure that your donor liver is delivered to you while it is still viable (within eight to nine hours).
It is preferred for donor to have compatible blood group (the same blood group that recipient has), but now a day’s incompatible blood group transplant (transplant with different blood group) is also possible. However, in this type of transplant, antibodies in the patient against donor blood group has to be removed through plasmapheresis/immunoadsorption/ Medication. So, this type of transplant is more costly as compared to transplant with same blood group. The donor and recipient will have to undergo detailed tests, which could take 7-15 days (depending on what is found on investigations), prior to transplantation. The Transplantation can be done if the recipient and donor are found to be fit after these tests. Incompatible Liver Transplant is called ABO-incompatible liver transplantation (ABOi LT) as well.
When you are notified that a liver from a deceased donor is available, you should go to your hospital right away. You will be examined to determine whether you are healthy enough for surgery.
Because general anaesthesia is used during liver transplant surgery, you will be sedated throughout the procedure.
During this type of procedure, surgeons place a number of tubes and IVs (Intravenous Catheters) in your body to perform specific function (such as delivering fluids and medicine, monitoring blood pressure, taking blood samples, helping your breath by ventilator tube, drain blood and fluid from around your liver and draining urine etc.) while you are unconscious. The tubes will be left in place for a few days following your surgery.
During liver transplant surgery, the surgeon will make a long incision across your abdomen first to get access to your liver. The location and size of the incision can vary depending on your surgeon's approach and your anatomy. The surgeon will then remove the diseased liver and replace it with a donor liver.
Your surgeon will then connect your blood vessels and bile ducts to the donor's liver. The surgery could take up to 12 hours depending on the severity of your condition.
After the new liver is in place, the surgeon closes the incision with stitches and staples. After that, you are taken to the intensive care unit to begin your recovery.
If you are receiving your new liver from a living donor, the surgery must be planned ahead of time in advance.
The donor is first operated on, and the portion of the liver for transplant is removed. Following that, surgeons remove the diseased liver, and the new donated liver portion is implanted in your body. Following that, they will connect your blood vessels and bile ducts to the new liver.
The transplanted liver portion in your body, as well as the portion left behind in the donor's body, regenerates and regrow quickly and can reach normal volume within a few weeks.
Other activity during the surgery such as anaesthesia, incision and installing tubes and IVs (Intravenous Catheters) etc. will be almost the same.
After your procedure, you may need to stay in the intensive care unit for a few days. Medical personnel will need to keep an eye on your condition and look for signs of complications. They will also test your liver function on a regular basis to look for signs that the new liver is functioning properly. After you are discharged from the intensive care unit, you will need to spend some time in a transplant recovery area.
Your transplant team can make a check-up schedule for you, and you may need to have blood tests several times per week. You will also need to take medications such as immunosuppressants for the rest of your life after the transplant. This medication prevents your immune system from attacking your new liver, and other medications can help reduce the risk of complications.
It could take up to six months to fully recover. The length of time required is also determined by the severity of your condition prior to the transplant. It is also critical to eat a well-balanced diet to aid recovery and maintain liver health.
Like most transplants, liver surgery carries a significant risk of complications, which are associated with both the procedure itself and the drugs required to prevent rejection of the donor's liver once the transplant is complete. Some of the risks associated with the procedure include:
If the complications are long-term, they may result in the recurrence of the liver disease in the transplanted liver.
To prevent your body from rejecting the new liver after a liver transplant, you will need to take medications for the rest of your life. However, these anti-rejection medications can have a variety of side effects, including:
Because anti-rejection drugs suppress the immune system, they increase the likelihood of infection.
Please note that this is general information about the liver transplant surgery, some details may change, if have any query please reach out to your liver transplant surgeon.